Charcot Foot and Ankle, also known as Charcot arthropathy or Charcot joint, is a condition caused by peripheral neuropathy, leading to the progressive degeneration and destruction of the soft tissue, joint, and bone. In modern society, the most common cause for this neuropathic neuropathy is diabetes mellitus, with long-term diabetic patients having an increased risk of developing the condition.
Given its progressive nature, a late Charcot Foot Diagnosis can lead to considerable morbidity, including potential limb loss. However, the clinical and radiological diagnosis of Charcot Foot and Ankle are both challenging. Furthermore, the clinical presentation of acute Charcot neuropathy and diabetic osteomyelitis is similar, and both conditions can co-exist in the same extremity, adding to the complexity of Charcot Foot diagnosis.
Although clinical history, risk factors, and physical and lab exams are important in the diagnosis of Charcot Foot and Ankle, imaging tools play a decisive role in arriving at the definitive diagnosis and adequate treatment. In this article, we will focus on the role of Computerized Tomography (CT) imaging in the diagnosis and management of Charcot arthropathy.
How to Use CT Scans to Diagnose Charcot Foot and Ankle
Although the use of CT scans in neuropathic arthropathy is not well investigated, this imaging tool has higher sensitivity for early intra-articular fractures that are not readily visualized in plain radiographs. CT can also show periosteal new bone formation and small foci of gas within bone in a better way than MRI can. Other findings that can be evidenced with the use of CT are cortical destruction, anatomical deformities, structural bone damage, fractures, subluxations, and bone callus formation.
When MRIs are contraindicated, the use of CT is particularly useful to visualize all bones of the foot, particularly the midfoot, which is difficult to see well on radiography and one of the crucial points of damage in Charcot Foot and Ankle.
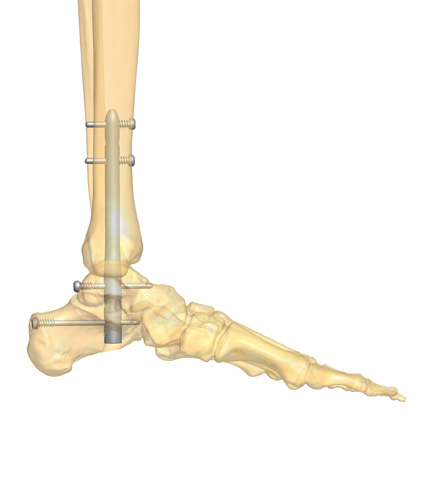
Currently, the most used CT scanning technique is the multidetector computed tomography (MDCT), and its use with reconstruction and three-dimensional (3D) computer-generated images from multiple planes is advantageous in preoperative planning and follow-up of immobilization therapy.
When using the MDCT to create 3D images, both feet should be scanned to determine bilateral deformities and differences between feet. To determine if there is subluxation of the tarsometatarsal joints, radiologists should evaluate the transverse and coronal planes of the foot.
In early stages, when Charcot Foot symptoms are easily mistaken with other conditions and radiological signs can be non-existent or very subtle, the use of MDCT enables the analysis of normal bone density, joint distension, existence of bony debris, joint disorganization and dislocation, collectively known as the descriptive “five D’s” of neuropathic arthropathy.
The Patients’ Role
Early diagnosis of Charcot Foot and Ankle may be difficult, as the presentation with swelling and erythema can be overlooked or mistaken with other conditions, such as cellulitis or erysipelas. The use of 3D CT scans can help radiologists to address the spatial orientation of the bones and joints, especially the subtle but complex midfoot and rearfoot joint alterations in early stages of Charcot arthropathy.
Since the alterations caused by Charcot Foot and Ankle may be initially elusive, it is important that they are detected as soon as possible. To accomplish this, the patient must be aware of his or her crucial role in the disease management by doing regular check-ups, carefully taking care of their feet, and promptly communicating any alteration to a member of their multidisciplinary healthcare team.
Failing to take preventative measures and delaying treatment can result in burdensome complications, such as pronounced foot deformity, ulcers, infection, and ultimately lead to limb amputation.
If you wish to help your patients know more about Charcot Foot and Ankle, its link with diabetes, and their key role in the management of their disease, we suggest downloading the Patient Informative Cards “Stand On Your Feet: A Program of Empowerment for Your Diabetic Foot Management.”

References
- Mautone M, Naidoo P. J Med Imaging Radiat Oncol 2015 Aug;59(4):395-402.
- Marmolejo VS et al. Am Fam Physician. 2018 May 1;97(9):594-599.
- Schoots et al Semin Musculoskelet Radiol. 2010 Sep;14(3):365-76.
- Rogers LC, Bevilacqua NJ. Clin Podiatr Med Surg 2008; 25: 263–274, vii.
- Ergen FB et al. Diabet Foot Ankle. 2013 Nov 20;4.