Charcot foot, also called Charcot neuropathy, is a condition caused by a combination of peripheral neuropathy and vascular disorders that results in progressive joint damage and eventually foot instability1. If left untreated, the consequences for patients are devastating, with reduced quality of life, inability to weight-bear, and an increased risk of amputation2.
The initial management of acute Charcot foot relies on offloading the affected foot to prevent further damage, either with a total contact cast, or alternatives such as the Charcot-restraint orthotic walker3. The aim is to preserve the soft tissue envelope by preventing or limiting the impact of any bony deformity that may occur4. Dr. Stephanie Oexeman, DPM, says: “I have a very low threshold for offloading to try and prevent as much damage and collapse of the foot.”
However, conservative Charcot foot treatment may not be enough, especially in more advanced stages, when patients present with a disabling deformity or severe instability5. The indications for Charcot foot surgery include3,6:
- Severe instability or arthropathy
- Failure of conservative methods to obtain a plantigrade foot
- Presence of long-standing ulceration or osteomyelitis
- Expected ability of the patient to use commercially available footwear after surgery.
The decision to embark on surgical treatment for Charcot foot should also take into account the patient’s characteristics and comorbidities, since it is not a risk-free intervention3.
This article highlights the various techniques for reconstructive and non-reconstructive surgery to treat Charcot foot, as well as what to expect in terms of complications and revision rates.
Charcot Foot Reconstruction
Recently, there has been a heightened level of interest in surgical reconstruction due to a combination of advancements in surgical instrumentation and fixation devices, along with contemporary evidence regarding long term outcomes4,7. The goal of Charcot foot reconstruction is to correct deformity to achieve a stable, plantigrade foot that allows for weight-bearing.
A range of techniques have been developed and described to obtain a plantigrade foot that can weight-bear, but it is difficult to identify a single technique and/or procedure that will be effective for all patients, given that patients with Charcot foot also have conditions such as diabetes, osteoarthritis, and/or vascular problems, which can complicate outcomes4.
The midfoot is the most frequently affected region by Charcot neuropathy, followed by the hindfoot and ankle8. Figure 1 illustrates a case of Charcot foot with excessive motion upon midfoot and hindfoot.

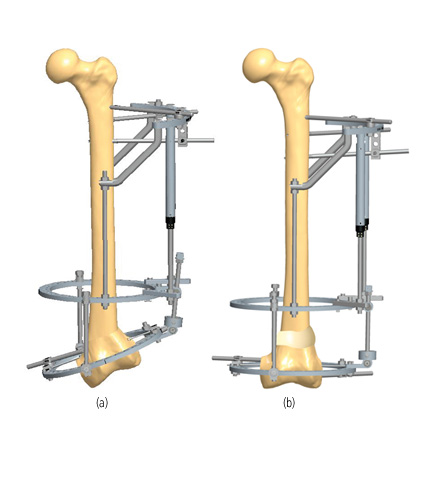
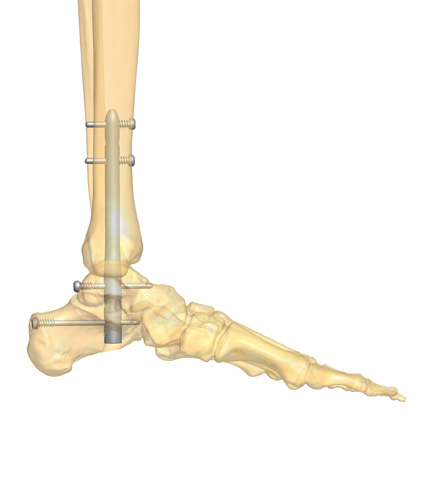
Surgical reconstruction is ideally performed during the quiescent stage of the disease process9. Since the goal is to achieve a biomechanically stable foot, surgical reconstruction often involves restoration of the normal alignment angles in the foot (Figure 2)9. However, it is important to not compromise the vascularity and soft tissue integrity of the foot in a quest to obtain perfect radiological angles9.

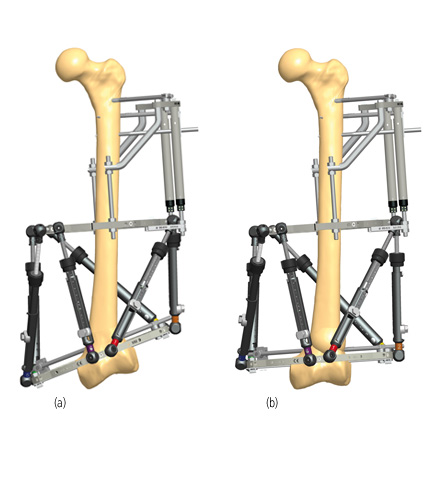
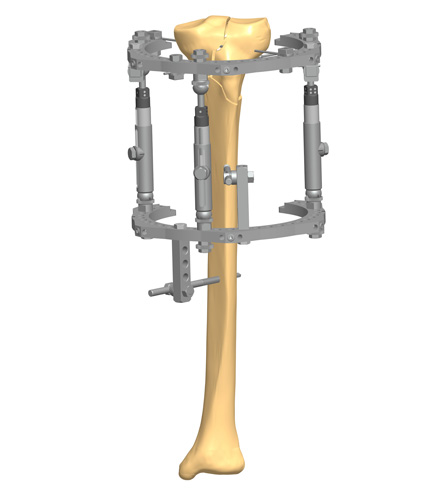
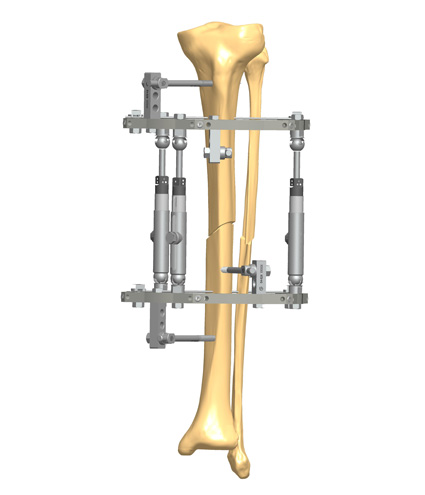
Surgical reconstruction of the deformed Charcot foot can be obtained with internal fixation, external fixation, or a combination of both, depending on patient characteristics and other factors, such as soft tissue integrity. For a detailed overview of the devices used in Charcot foot surgery, read our article on surgical approaches.
In an article detailing the cost-effectiveness of various treatment strategies for Charcot foot, Albright et al. showed that the most effective strategy for patients without foot ulcers or with uninfected ulcers was reconstruction, which resulted in an additional 1.63 or 1.04 quality-adjusted life-years gained compared with lifetime bracing10.
Complications of surgical reconstruction of Charcot foot include delayed healing, dehiscence, and major lower extremity amputation, especially in patients with vascular problems and diabetes11. The presence of peripheral arterial disease increased the risk of delayed healing by more than 2-fold, and increased the risk of major lower extremity amputation by 4.41-fold, highlighting the need for a careful vascular evaluation prior to a planned surgical intervention11.
Charcot Foot Non-reconstructive Surgery
Ideally, every collapsed or deformed Charcot foot would be surgically transformed into a stable and ambulatory limb segment, but unfortunately not all patients can undergo major reconstructive surgery7. Furthermore, the patient’s healing capacity is a major predictor of outcomes, so it is important to carefully select the patients that have the most potential to benefit from each surgery.
“The decision on the surgical technique depends on the underlying biomechanics and the progression of the deformity. Tendon lengthening and tenotomies can be powerful tools to achieve a braceable foot. However, in the presence of osseous deformities, reconstruction is the preferred option.” — Dr. Stephanie Oexeman, DPM, Oexeman Foot and Ankle, Chicago.
Apart from reconstruction, common surgical interventions for Charcot foot include ulcer debridement and exostectomy of bone prominences4. The typical rocker-bottom deformity associated with midfoot Charcot foot (Figure_3) can cause pressure and mechanical stress on the tissues that cover the exostosis, eventually leading to ulceration12. Consequently, soft tissue surgical interventions are often a standard approach to manage pressure imbalances in a Charcot foot13.

Non-infected, acute ulcers may be treated with local debridement, but recalcitrant, large chronic ulcers in high-pressure areas may require more aggressive surgical debridement in the operating room, as well as those with concomitant soft tissue or bone infection7.
Surgical ostectomy or exostectomy of areas with bony prominences are a non-reconstructive method to relieve pressure and allow for ulcer healing7. When deciding to perform this procedure, the most important factor to consider is the patient’s foot stability. Those patients with major instability may not benefit and may be harmed by further bone excision, resulting in further instability and collapse7.
Other non-reconstructive surgical options include7:
- Muscle flaps may be used to provide soft tissue coverage, with the advantage of providing vascularity
- Equinus correction, through Achilles tendon lengthening, gastrocnemius recession, or a complete tenotomy
- Correction of residual varus deformities, through tibialis anterior and tibialis posterior tendon transfers.
Unfortunately, despite surgeons’ best efforts, there are instances when even surgical management fails, and amputation must be considered. It is indicated in cases of unstable arthrodesis, recurrent ulceration, refractory infections, and cases in which the patient is unlikely to ambulate on their own or benefit from other procedures14-16. Amputation may be performed at various levels, but transtibial is usually preferred, if possible, since it facilitates prosthetic fitting7,17.
Choosing the right surgical approach for a Charcot foot is unquestionably a challenge for the orthopedic specialist17. Become a subscriber to gain more insight and access a series of Charcot Foot Reconstruction Case Reports, available here.

References
1. Hester T, Kavarthapu V. Etiology, Epidemiology, and Outcomes of Managing Charcot Arthropathy. Foot and Ankle Clinics. 2022/09/01/ 2022;27(3):583-594. doi:https://doi.org/10.1016/j.fcl.2022.03.002
2. Wukich DK, Sung W, Wipf SAM, Armstrong DG. The consequences of complacency: managing the effects of unrecognized Charcot feet. Diabetic Medicine. 2011;28(2):195-198. doi:https://doi.org/10.1111/j.1464-5491.2010.03141.x
3. Schmidt BM. Clinical insights into Charcot foot. Best Pract Res Clin Rheumatol. Jun 2020;34(3):101563. doi:10.1016/j.berh.2020.101563
4. Ha J, Hester T, Foley R, et al. Charcot foot reconstruction outcomes: A systematic review. J Clin Orthop Trauma. May-Jun 2020;11(3):357-368. doi:10.1016/j.jcot.2020.03.025
5. Galhoum AE, Trivedi V, Askar M, et al. Management of Ankle Charcot Neuroarthropathy: A Systematic Review. Journal of Clinical Medicine. 2021;10(24):5923.
6. Salvaterra P. The Surgical Management of Neuropathic (Charcot) Foot – A Practical Guideline. 2017;
7. Chen S, Miller JD, Steinberg JS. Management of the Charcot Foot and Ankle: Nonreconstructive Surgery. Clinics in Podiatric Medicine and Surgery. 2022/10/01/ 2022;39(4):559-570. doi:https://doi.org/10.1016/j.cpm.2022.05.003
8. Rosemberg DL, Sposeto RB, Godoy-Santos AL. Arthrodesis in the Deformed Charcot Foot. Foot and Ankle Clinics. 2022/12/01/ 2022;27(4):835-846. doi:https://doi.org/10.1016/j.fcl.2022.08.005
9. Kavarthapu V, Vris A. Charcot midfoot reconstruction—surgical technique based on deformity patterns. Annals of Joint. 2020;5
10. Albright RH, Joseph RM, Wukich DK, Armstrong DG, Fleischer AE. Is Reconstruction of Unstable Midfoot Charcot Neuroarthropathy Cost Effective from a US Payer’s Perspective? Clinical Orthopaedics and Related Research®. 2020;478(12)
11. Cates NK, Elmarsafi T, Akbari CM, et al. Complications of Charcot Reconstruction in Patients With Peripheral Arterial Disease. The Journal of Foot and Ankle Surgery. 2021/09/01/ 2021;60(5):941-945. doi:https://doi.org/10.1053/j.jfas.2019.08.039
12. Laurinaviciene R, Kirketerp-Moeller K, Holstein PE. Exostectomy for chronic midfoot plantar ulcer in Charcot deformity. Journal of Wound Care. 2008/02/01 2008;17(2):53-58. doi:10.12968/jowc.2008.17.2.28178
13. Botek G, Figas S, Narra S. Charcot Neuroarthropathy Advances: Understanding Pathogenesis and Medical and Surgical Management. Clinics in Podiatric Medicine and Surgery. 2019/10/01/ 2019;36(4):663-684. doi:https://doi.org/10.1016/j.cpm.2019.07.002
14. Schon LC, Bae S-Y, Mousavian A. Procedure 27 – Charcot Neuroarthropathy of the Midfoot. In: Pfeffer GB, Easley ME, Hintermann B, Sands AK, Younger A, eds. Operative Techniques: Foot and Ankle Surgery (Second Edition). Elsevier; 2018:216-228.
15. Güven MF, Karabiber A, Kaynak G, Öğüt T. Conservative and surgical treatment of the chronic Charcot foot and ankle. Diabetic Foot & Ankle. 2013/01/01 2013;4(1):21177. doi:10.3402/dfa.v4i0.21177
16. Pinzur MS. Surgical treatment of the Charcot foot. Diabetes/Metabolism Research and Reviews. 2016;32(S1):287-291. doi:https://doi.org/10.1002/dmrr.2750
17. Galli M, Scavone G, Vitiello R, Flex A, Caputo S, Pitocco D. Surgical treatment for chronic Charcot neuroarthropathy. The Foot. 2018/09/01/ 2018;36:59-66. doi:https://doi.org/10.1016/j.foot.2018.02.001